September 7, 2024
Incontinence Treatment
Physical Rehabilitation In Women With Urinary Incontinence Overall closure rates after medical fixing of vesico-vaginal fistulae range from % [706] During the stepping in period in between medical diagnosis and repair, UI pads with the aim of prevention of skin issues related https://Achievable-wellness.b-cdn.net/Achievable-wellness/pelvic-floor-therapy/surgical-treatments-for-females-with-tension-urinary-system-incontinence-a.html to chronic urinary leakage can be given and making use of an obstacle lotion or regional oestrogen can additionally be taken into consideration [704,705] An injury to the urinary system throughout hysterectomy for benign conditions (60-- 75%), hysterectomy for malignant conditions (30%) and caesarean area (6%) are the primary causes of postoperative VVF in the developed globe [676,677]- One small test discovered 30% (six out of 20) of patients established retention of urine complying with peri-urethral shot compared to 5% (one out of 20) with transurethral injection [374]
- If you do not accept the conditions, you might not access or make use of software.
- Requirement standard, gold requirement-- Criterion criterion is an examination thought about to be the diagnostic criterion for a specific illness or problem, made use of as a basis of contrast for various other (typically noninvasive) tests.
- Growth computer system registry data were supplemented by medical facility document and histologic evaluation searchings for in men aged 55 to 74 years with clinically localized prostate cancer cells.
- Description of individuals as being of a regional descent (eg, of African, Asian, European, or Middle Eastern or North African descent) is acceptable if those terms were made use of in official research study.
Sorts Of Pressure Transducers
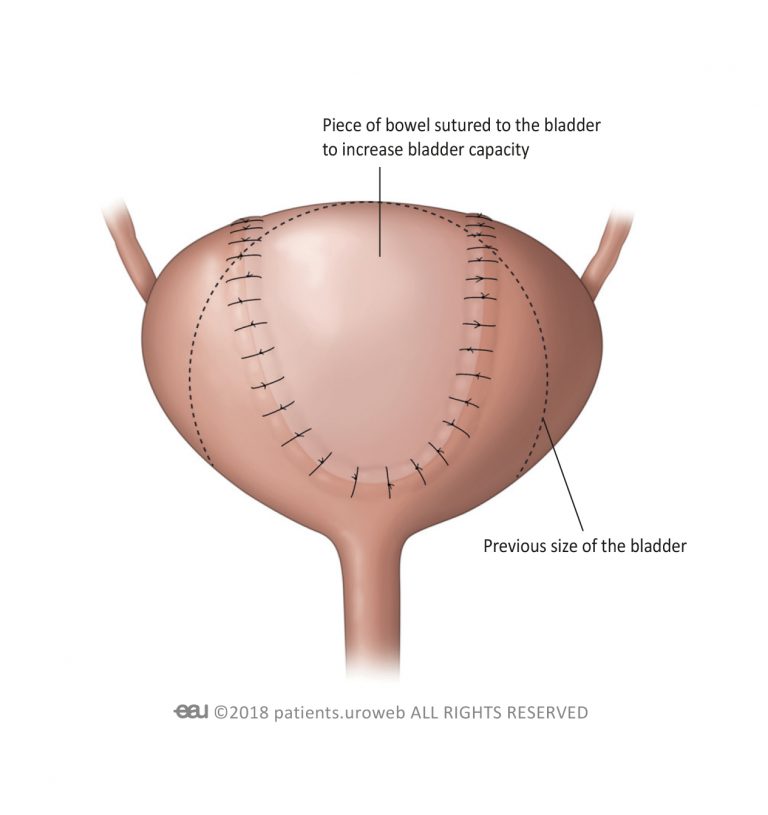
Valsalva leakage point stress did not dependably evaluate incontinence severity in an accomplice of ladies picked for surgical treatment of SUI [69] Procedure post-void residual (PVR) quantity, particularly when assessing patients with nullifying signs and symptoms or difficult anxiety urinary incontinence (SUI). Urinary system diversion continues to be a reconstructive choice for patients with intractable UI after numerous pelvic procedures, radiotherapy or pelvic pathology causing permanent sphincteric incompetence or fistula development. Choices consist of ileal conduit urinary system diversion, orthotopic neobladder and heterotopic neobladder with Mitrofanoff continent catheterisable conduit. There is insufficient evidence to talk about which procedure causes the most enhanced QoL.Male Incontinence: A Complete Guide To Wearable Solutions
A large evaluation found similar outcomes, and the continence rates for open Burch treatments were kept in mind to be 85% at 1 year postoperatively and around 70% after 5 years [31] Midurethral sling entails placing a strip of artificial mesh via the retropubic room or obturator foramen. Transobturator (TODDLER) was created to reduce the possible threat for bladder injuries and is thought about to be the safer of the two choices due to the fact that, unlike TVT, it stays clear of a medical approach in between the pubic bone and the bladder. A search of the literary works was centered on the 3 most typical medical methods, consisting of the midurethral sling, Burch colposuspension and autologous pubovaginal sling.What is a significant risk factor of urinary incontinence?
Social Links